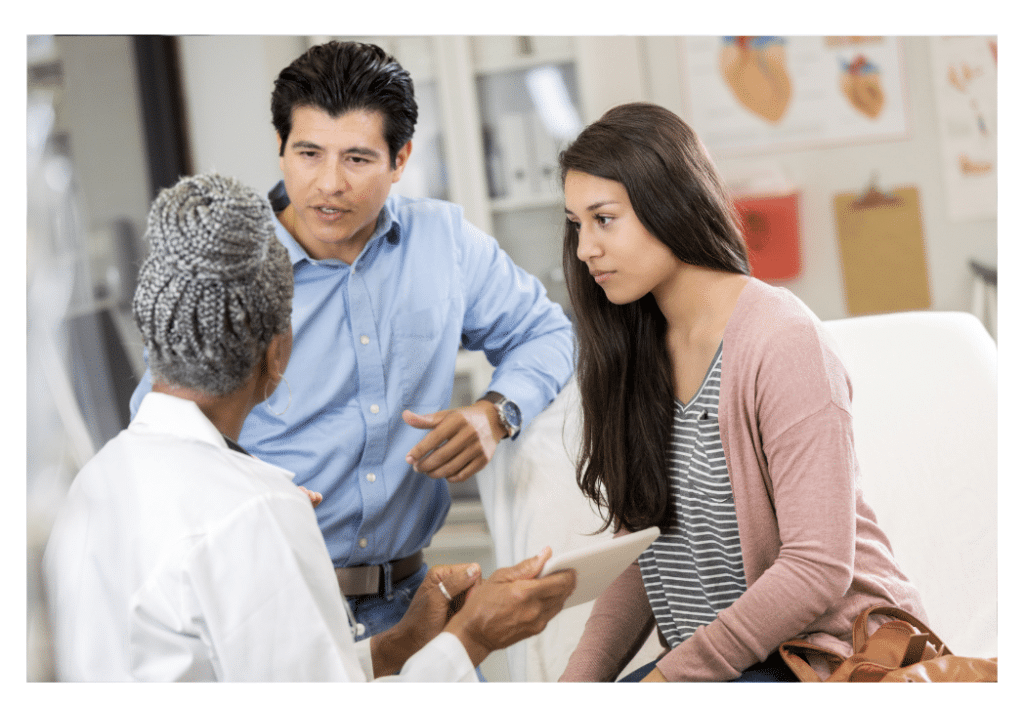
As an intended parent or potential gestational carrier, deciding to pursue surrogacy can feel overwhelming. It’s natural to wonder about the similarities and differences between the types of surrogate pregnancies, the legalities, obligations, and the actual process of growing a baby or having someone grow a baby for you. Join us for Surrogate Pregnancy 101.
TRADITIONAL SURROGACY PREGNANCY
There are two primary types of surrogate pregnancies. The less common option is traditional surrogacy. While less complicated from a procedural perspective, it’s often not the preferred choice as one (or both) intended parents will not have a biological connection to the baby.
Traditional surrogacy is when a gestational carrier’s egg is fertilized by an intended parent’s sperm or a sperm donor. The method is called “intrauterine insemination (IUI),” as sperm cells are injected directly into the surrogate’s womb during ovulation. In other words, the embryo comes from the surrogate’s egg and sperm from the intended father or a donor.
From a legal standpoint, a traditional surrogate is still viewed as a mother since she has a biological connection to the child. Therefore, traditional surrogacy involves an extensive legal process to terminate the surrogate’s parental rights, then having the non-biological parent legally adopt their baby.
GESTATIONAL SURROGACY: WHAT IS IVF?
The second type of surrogate pregnancy is gestational surrogacy. This is the most common and sought-after type of surrogate pregnancy, as it’s more likely that both intended parents will have a genetic connection to the baby. The gestational carrier will have no genetic tie to the baby whatsoever. While this type of surrogacy is preferred, the process is more complex than a traditional surrogate pregnancy as it requires in-vitro fertilization (IVF), a process with many carefully timed steps that we’ll outline below.
Pennsylvania, New Jersey, and Delaware all have favorable legal environments for gestational surrogacy. The gestational carrier has no claims to parental rights. Therefore, before the baby is born, the Intended Parent(s) are reaffirmed as the baby’s sole legal parent(s) through a simple parentage action. This is often called a pre-birth order.
THE IVF PROCESS

In vitro means “in a test tube, culture dish, or elsewhere….” At a high level, in-vitro fertilization, or the IVF process, is when an egg is fertilized with sperm in a lab. After fertilization, it grows into an embryo, which is then implanted into the surrogate or gestational carrier’s uterus. This may seem simple, but as we said before, many steps are involved in the IVF process. So, let’s take a closer look, shall we?

STEP 1: PREPARATION & EMBRYO CREATION
Before Intended Parents begin the matching process for a surrogate, they will create embryos through IVF. The fertility doctor will work with the Intended Mother or an egg donor to screen her overall health and check hormone levels. This is to ensure she’s physically ready for superovulation.
STEP 2: HORMONE THERAPY
STEP 3: EGG RETRIEVAL AND FERTILIZATION
Once the egg cells and sperm are ready to go, it’s time for fertilization. This involves mixing the eggs and sperm in a lab dish or test tube. While several technologies are used for the fertilization process, the most common choice is intracytoplasmic sperm injection (ICSI).
To ensure most of the egg cells were properly fertilized, an embryologist will monitor the progress of what they believe are fertilized egg cells. They are focusing on the embryo cell division process from 2 to 4 to 8 to 16 cells. They are also monitoring the health of the embryos. When the embryos have reached 100 to 150 cells, they’ll determine which embryos are most viable for transfer. The evaluation part of the process could take up to 5 days.

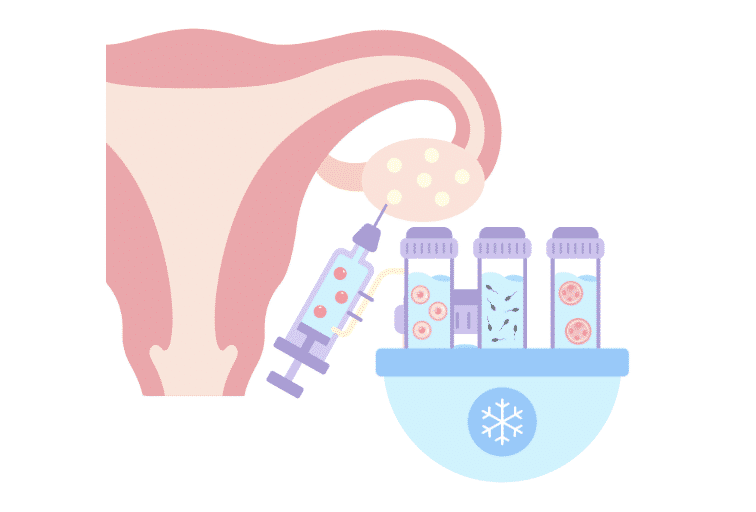
STEP 4: TESTING AND FREEZING
Once embryos have been created, they can be biopsied for further genetic testing. This testing is optional but can identify chromosomal abnormalities and other genetic issues. The embryos are then frozen for storage using a process called vitrification. Freezing embryos keep them perfectly stable and ready for thawing at a later date for transfer into a surrogate.
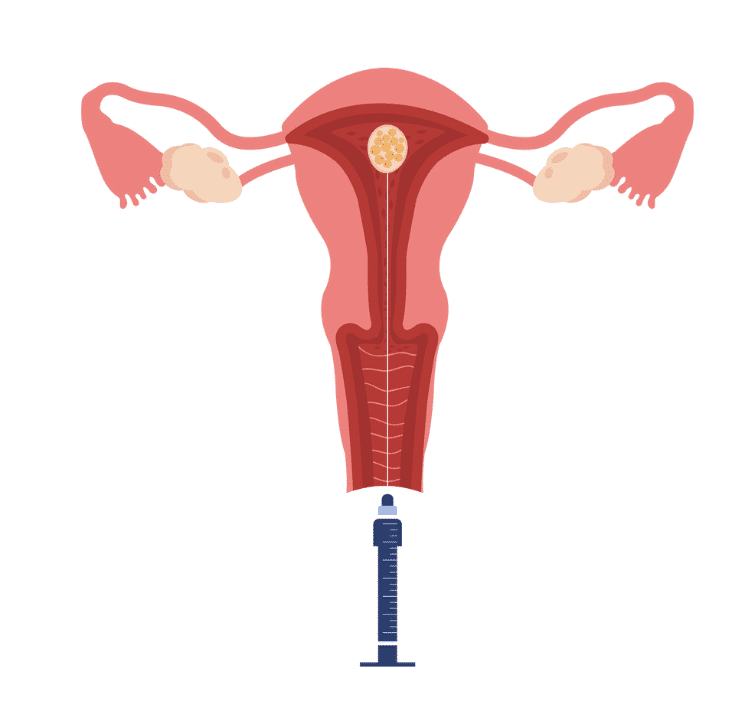
STEP 5: EMBRYO TRANSFER, IMPLANTATION, AND PREGNANCY
While simple, the embryo transfer process is the most delicate step in IVF. The fertility doctor inserts a tiny catheter into the surrogate’s uterus through the cervix under ultrasound guidance. The procedure is not uncomfortable and takes only a few minutes!
Once the catheter is in place, the fertility doctor will inject the embryo(s) into the surrogate’s uterus. The embryo(s) are expected to attach to the uterine wall and continue to grow.
After ten days, the fertility clinic will confirm the pregnancy. This will be done with a blood test to ensure maximum accuracy. At least two blood tests will check for HCG hormone in the surrogate’s blood. If these numbers exceed 50mIU/ML, an ultrasound will be scheduled two weeks later. A fetal heart rate cannot be confirmed yet. Still, an ultrasound will confirm that initial fetal development looks normal and that the embryo has not migrated to other parts of the uterus (i.e., an ectopic pregnancy). A fetal heart rate can typically be confirmed five or six weeks after the transfer, and the surrogate is declared pregnant.
WHAT IF THE EMBRYO TRANSFER FAILS?
Above, we shared the importance of ovarian stimulation and harvesting at least 10-15 eggs. This is because not all eggs are suitable for fertilization, and of those that are fertilized, not all will grow into healthy embryos. Embryo quality is the main determining factor of overall success rates for surrogacy. Intended parents should aim for at least two or three embryos for use in gestational carrier cycles.
If an initial embryo transfer fails, additional attempts can be made. The gestational carrier agreement outlines and agrees upon the number of attempts to be made. Most fertility specialists believe three unsuccessful attempts should be the limit with a single carrier. As a point of reference, the success rate for the first transfer is about 60%, with about 80% of surrogates getting pregnant within two transfer attempts.
ROLE OF SURROGACY AGENCY
The role of a surrogacy agency like the Surrogacy Center of Philadelphia is that of a facilitator. Our responsibility is to match surrogates with intended parents and get everything memorialized in a contract. We then coordinate activities between the fertility clinic, intended parents, and surrogates.
Please reach out if you’d like to learn more about the surrogacy process or how our agency can help. We’d be happy to help navigate this journey with you!